© 2024 Apreva Hospice
All Rights Reserved
All Rights Reserved
Everyone knows about heart attacks… but have you ever heard of atrial fibrillation? Despite being the most common heart arrhythmia (meaning irregular heartbeat) that is medically treated and being the cause for 1 in 7 strokes, most people aren’t familiar with atrial fibrillation. Surveys have revealed that even those who are aware of it often don’t consider it a serious medical condition. Education is key here, as leaving atrial fibrillation untreated doubles the risk of heart-related deaths and increases the risk of having a stroke significantly. It is estimated that by 2030, about 12.1 million people living in America will have a diagnosis of AFib. Considering how high that number is, it’s time to start paying attention to what it is and how you can mitigate yours and your loved ones’ risk factors!
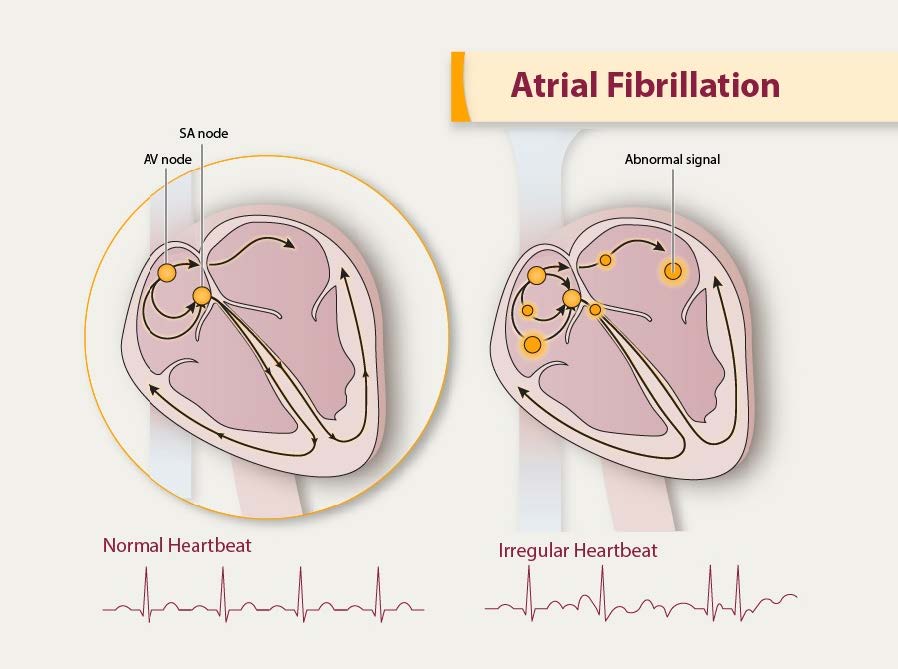
So what is atrial fibrillation? Atrial fibrillation, abbreviated AFib, is an abnormal heart rhythm during which the top chambers of your heart, called your atria, quiver rather than beat, leading to inefficient movement of blood through your heart. Given the inefficient contraction of the heart, individuals with AFib are at a higher risk for clots. The higher risk of clotting and the decreased ability of the heart to pump blood efficiently is what leads to an increased risk of further heart conditions and stroke should a clot form and travel to the brain.
While some individuals with AFib might not know they have it and may experience no symptoms at all, others could experience a number of various symptoms. Pay attention to the symptoms and take action. Consider scheduling an appointment with your doctor if you or a loved one are experiencing any of the following:
In addition to symptom monitoring, there are a number of risk factors to be aware of related to AFib. Considering the risk of stroke and heart disease increases significantly with AFib, mitigating the risk factors of AFib is crucial. Risk factors include:
If any of these risk factors apply to you or a loved one, consider if your risk factors are modifiable, meaning you have more control over reducing how much of a risk they pose. Focus on lowering your blood pressure, losing weight if appropriate, reducing or eliminating alcohol intake and quitting smoking. Consuming whole, natural foods when possible, incorporating exercise and purposeful movement every day, and staying hydrated can go a long way in preserving your health!
If you have already been diagnosed with AFib, it is important to continue to mitigate as many risk factors as you can using the guidance above, in addition to seeking proper medical treatment for your condition. Lifestyle changes, even after being diagnosed with AFib, can greatly decrease the severity and frequency of your symptoms. These lifestyle changes include cutting back on alcohol, reducing caffeine, quitting smoking, exercising regularly, eating a nutrient rich diet, losing weight if required and lowering your blood pressure. When prescribed medications for AFib, especially blood thinners to reduce the risk of clots, it is imperative that you follow the guidance of your doctor and stay consistent with the treatment.
Given that AFib is a chronic condition, meaning it doesn’t go away, it is likely that you will be on medication to manage it for the rest of your life. This can be scary and anxiety inducing if you don’t understand your medications or don’t have a plan to stay on track. Meet with your doctor and be sure to understand what medications you are taking, why you are taking them, how long you will be taking them for and what side effects to look out for. You deserve to understand and feel comfortable with your treatment, so be sure to collaborate with your medical team and find support from your loved ones.
Atrial fibrillation – if it’s not taken seriously, it could cause serious problems!
Know the symptoms, schedule regular visits with your doctors, and practice a healthy lifestyle to reduce your risk!
Image 1 – https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
Image 2 – https://www.mcrmedical.com/blog/aha-2020-guidelines/
Heart Foundation –
https://www.heartfoundation.org.nz/your-heart/hearthelp/atrial-fibrillation/managing-your-af
CDC – https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
American Heart Association –https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af
When you hear the word “diabetes”, chances are it hits home on some level. It may be a loved one, a parent, a friend, or yourself who is living with this disease. They are just one of 34 million Americans living with a diabetes diagnosis. Another 96 million have prediabetes. Of those 96 million, 80% of them do not know they have prediabetes, highly increasing the likelihood of developing diabetes down the road. The consequences of this disease are high, and the prevalence across our population is increasing. November is American Diabetes Month, a month dedicated to raising awareness about how to prevent diabetes and improving the resources available to those living with it.

There are three different types of diabetes that contribute the most to the diabetes epidemic. They include prediabetes, type 1 diabetes, and type 2 diabetes. Though they are all a bit different from one another, all forms of diabetes are related to insulin and blood sugar levels. Insulin is a hormone released by the pancreas and its job is to regulate the levels of glucose, also known as sugar, in your bloodstream.
Type 1 diabetes, also known as “insulin dependent” diabetes, is an autoimmune disorder during which the cells of the pancreas that produce insulin are destroyed. When these cells are destroyed, the body cannot produce insulin. This results in glucose staying in the bloodstream rather than being taken up by the cells in your body. Over time, this causes blood sugar levels to rise without the body having a way to naturally regulate them back down to normal. Individuals with type 1 diabetes are often diagnosed during childhood or adolescence, though it is possible for adults to develop type 1 diabetes. The treatment for type 1 diabetes must involve taking insulin every day because the body cannot make it and checking blood sugar levels regularly throughout the day. Consuming a healthy, balanced diet and partaking in regular exercise should be included in the management of type 1 diabetes to help avoid complications.
Type 2 diabetes, also known as “insulin resistant” diabetes, is caused by the body not producing sufficient amounts of insulin or the body resisting the insulin being produced. In both cases, the body is unable to properly regulate blood sugar levels. The biggest risk factors for developing type 2 diabetes are obesity and high blood pressure. In the past, you would see this type develop most often in adults over 45. In recent years, the number of children and teens developing type 2 diabetes has been increasing as a result of poor nutrition and rise in obesity. Due to the nature of type 2 diabetes, it can be successfully managed through a healthy diet, regular exercise, and maintaining a healthy weight. In some cases, when lifestyle changes aren’t sufficient, type 2 diabetics must supplement with oral medications and insulin to help control blood sugar levels.
When blood sugar levels are higher than normal but not high enough to be classified as diabetes, it is called prediabetes. While prediabetes isn’t technically classified as diabetes, it often develops into a full diagnosis of diabetes if no intervention is implemented. Awareness is the key to success here as many individuals may not develop symptoms until it is too late. Lifestyle changes that are implemented by individuals with prediabetes can often prevent or drastically delay the development of type 2 diabetes. These lifestyle changes include following a diet of minimally processed foods and regularly partaking in exercise.
If you or a loved one have already been diagnosed with diabetes or you suspect you may be at risk, schedule an appointment with your doctor to share your concerns and maintain regular checkups. Without proper care, serious complications such as hypoglycemia (low blood sugar), kidney failure and heart disease can occur. Preventing these complications requires adherence to treatment per your doctors’ guidelines, a healthy diet and regular exercise.
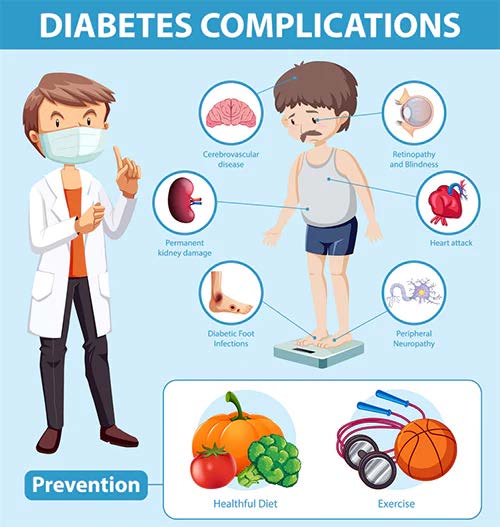
Diabetes is widespread across America, but it is not an insignificant diagnosis. This disease must be taken seriously and treated properly in order to avoid complications. Unfortunately, not everyone has equal access to the medical resources and education that makes living a normal and fulfilling life with diabetes possible. Raising awareness and equalizing care is one of the major goals throughout the month of November. We encourage you to take the time this month to share this article with family, friends and loved ones. Encourage those around you to speak up about the risk and prevalence of diabetes in our communities. The more we open up the discussion about diabetes, the more we can band together in order to support our loved ones and improve the health of our community.
Visit The American Diabetes Association to learn more or to offer a donation towards ending diabetes. https://diabetes.org/
Image 1 – https://newatlas.com/medical/type-2-diabetes-protein-beta-cell-protection/
Image 2 – https://www.diabeticwarehouse.org/blogs/articles/diabetes-complications
American Diabetes Association – https://diabetes.org/
CDC – https://www.cdc.gov/diabetes/library/spotlights/diabetes-facts-stats.html
Endocrine Society –
https://www.endocrine.org/patient-engagement/endocrine-library/diabetes-and-older-adults
National Institute on Aging – https://www.nia.nih.gov/health/diabetes-older-people
Speare Memorial Hospital –
https://spearehospital.com/november-is-american-diabetes-month/# World Health Organization – https://www.who.int/news-room/fact-sheets/detail/diabetes
Think back through your lifetime, and you can likely recall a time during which you experienced an infection. Virtually everyone has. We often brush off the minor ones, such as a small cut from gardening or a burn from cooking dinner, either of which could become infected. We also occasionally are burdened with the more serious ones, like appendicitis or pneumonia, which tend to force our attention. The truth is though, almost every infection can lead to sepsis, even the ones that start off as seemingly no big deal. In recognizing how common infections are, it is imperative that we understand what sepsis is, who is susceptible, and how it can be prevented and treated in order to save lives.
Sepsis occurs when the body begins to damage its own tissues in response to an already existing infection. This can become life-threatening as the inflammation becomes widespread and blood clotting reduces blood flow. When sepsis is prolonged without treatment, it turns into septic shock. Septic shock is characterized by a severe drop in blood pressure leading to organ damage and death.

Although anyone can get sepsis (remember, it starts with an infection, and almost everyone gets one, if not many, infections throughout their lifetime), there are certain populations that are more susceptible. These populations include the very old (sixty-five years and above), the very young, pregnant women, patients being hospitalized, and individuals with pre-existing infections and medical conditions. These individuals already have compromised or altered immune systems, making it much harder for the body to fight off infections, even ones that may seem minor. The inability to fight off the initial infection leads to widespread inflammation and blood clotting.
Though serious and frightening, sepsis is not rare. Approximately 1.7 million Americans are diagnosed with sepsis yearly. Roughly 30% of individuals diagnosed with sepsis do not survive. One in three patients in the hospital who acquire sepsis die. Though sepsis requires immediate medical care, the infection that causes sepsis starts outside of the hospital in nearly 87% of cases.
Because infections that develop into sepsis often start outside of the hospital, it is important to recognize which ones have the potential to do so and what the best prevention measures are. Sepsis is most commonly caused by bacterial infections, but can also result from fungal, viral or parasitic infections. Common types of infections that lead to sepsis include infections of the abdomen, such as appendicitis or peritonitis, infections of the central nervous system, infections of the lungs, such as pneumonia, infections of the skin, and infections of the urinary tract, such as urinary tract infections (UTIs). Some of these infections are harder to recognize than others. General sepsis prevention measures to practice at all times include good hand hygiene, keeping cuts, wounds and burns clean, staying up to date on recommended vaccines, seeking routine medical care, especially for chronic conditions, and seeking medical support for suspected infections, especially if you or a loved one fall into one of the susceptible populations.
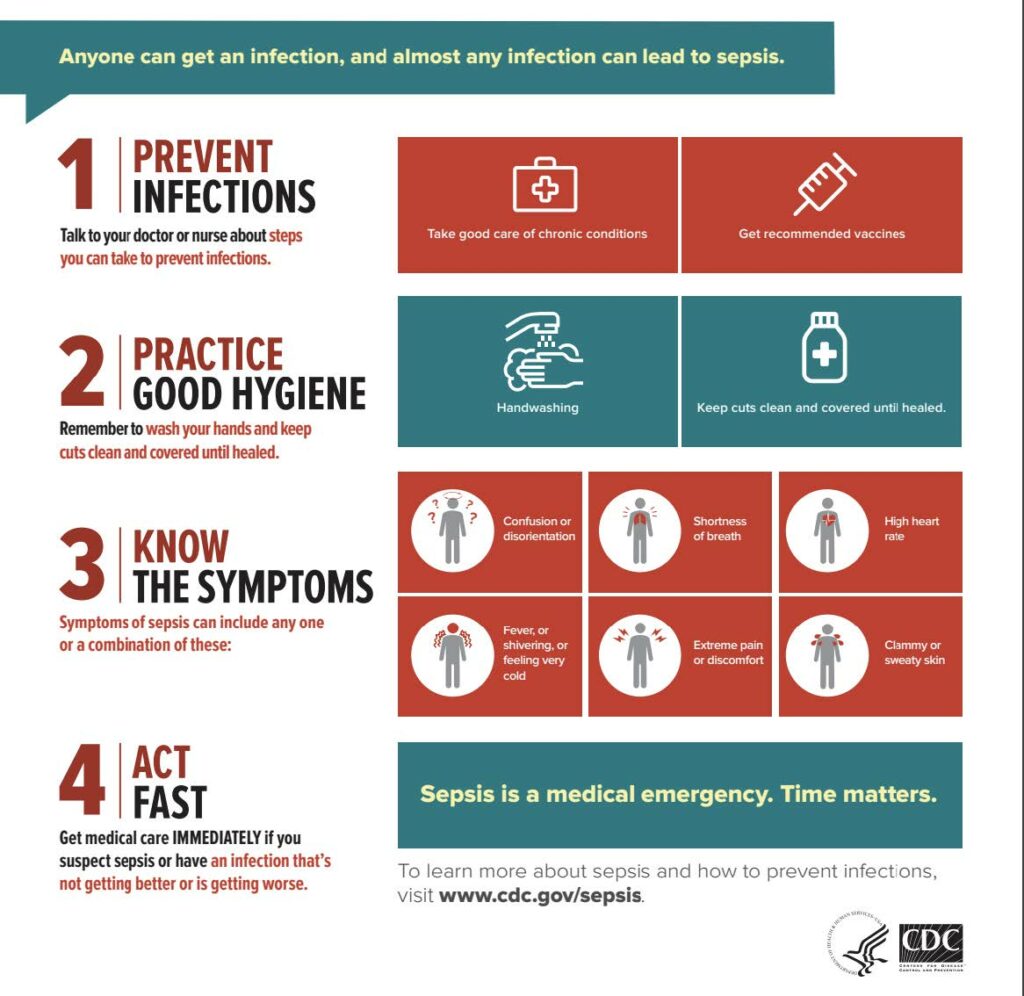
Though prevention is key, signs and symptoms of sepsis are important to recognize so you can seek immediate treatment should you experience them. They include high heart rate and low blood pressure, fever or hypothermia (low body temperature), shaking, chills, clammy skin, disorientation or confusion, and hyperventilation (fast breathing) or shortness of breath. Quick diagnosis and treatment is crucial for improving survival rates, so these signs and symptoms must be taken seriously and addressed immediately. If you or a loved one experience any of these symptoms, find in-person medical treatment or at a minimum, call your doctor with your concerns for further guidance.
Infections are common and must be taken seriously due to the risk of sepsis. Remember to practice your prevention measures and be diligent about seeking treatment should you suspect you are experiencing symptoms that could point to sepsis.
Image 1: https://www.cdc.gov/sepsis/what-is-sepsis.html
Image 2:
Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/12361-sepsis
Mayo Clinic:
https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
CDC: https://www.cdc.gov/sepsis/prevention/index.html

We all grieve differently, but one thing remains true for everyone: the importance of taking care of yourself. Whether you’ve found yourself in a state of just going through the motions or you’ve put all your focus on taking care of your loved ones, it can be easy to put your own needs on the back burner when facing the loss of a loved one.
However, it’s absolutely imperative that you take time to focus on yourself, too. In honor of Mental Health Awareness Month, we are discussing the importance of self-care throughout the grieving process.
Mental Health Awareness Month dates all the way back to 1949 when the National Association for Mental Health (now known as Mental Health America) first organized the observance in the month of May to help raise awareness and lessen the stigma attached to mental illness.
For a long time, society looked at mental illness as being just one thing. There was always a negative stigma attached to the term, and people often thought of those living with a mental illness as having ‘gone mad’. However, that is simply not true. Over time, we’ve learned more about the many layers and types of mental illness.
Mental illness is the term used to describe mental health conditions that impact a person’s mood, thinking, and behavior. Common mental illnesses include:
Losing a loved one can be a traumatic experience. You may feel as though you lost a part of yourself and that your life will never be the same. While there is some truth to this, it’s important to remember that you are still here and must go on living your life.
“We don’t move on from grief. We move forward with it.”
– Nora McInerny
Feelings of sadness, anger, loneliness, and hopelessness are all common throughout the grieving process. However, these feelings can sometimes develop into chronic grief which can in turn become a mental illness. In some cases, grief can lead to depression.
Symptoms of chronic grief can include:
Self-care used to be thought of as bubble baths and pampering yourself, but there is much more to self-care. Just like the grieving process, self-care can look different for everyone. But the overall concept is to take care of yourself physically, mentally, and emotionally.
To take care of yourself physically is pretty simple: eat a well-balanced diet, drink plenty of water, exercise regularly, and practice healthy hygiene habits. However, taking care of yourself mentally is a little less cut and dry. This is where it really differs from person to person. To take care of yourself mentally and emotionally, you need to take time to do the things that make you feel good and happy. Hobbies are a good place to start when focusing on taking care of yourself mentally. Maybe you enjoy sitting outside and reading a good book, maybe you are an artist, maybe you enjoy taking long walks with your dog. Whatever it is that leaves you feeling happy and fulfilled, do it!
Research shows the more you practice self-care, the more confident, creative, and productive you are. This also leads to experiencing more joy, making better decisions, building stronger relationships, and communicating more effectively. Overall, you will be in a better frame of mind, making you a better version of yourself. This is not only good for you, but it’s also good for those who depend on you.
When you take time to take care of your whole self (physically, mentally, and emotionally), it will help you to process your feelings of grief in a healthier way.
Always remember that you do not have to face the journey of grief alone. Lean on friends and family to help you through. Don’t be afraid to talk about your feelings. Sometimes we feel the need to be strong for those around us. If this is the case and you would feel more comfortable talking to someone outside the family, lean on the support of your hospice bereavement team. Our kind, compassionate bereavement coordinators are always available to talk or just listen. Never hesitate to reach out.
If you or someone you love is struggling with their feelings of grief and would like to talk to one of our bereavement coordinators, please contact us at (619) 450-4414.

By: Anonymous
May is Asian American and Pacific Islander (AAPI) Month, a time to learn about and celebrate the rich histories and cultures of Americans from the Asian continent and the Pacific Islands. The AAPI population is remarkably diverse, with 24 million people tracing their roots to over 30 countries. Many different cultures mean many different beliefs and traditions regarding the passage from life to death.
Demographic research reveals that AAPI Americans are less likely to access hospice and palliative care than other groups. Asian Americans, for example, have been shown to use fewer end-of-life services. Studies attribute this to cultural beliefs, language barriers, attitudes about death, and family-centered decision-making. But good hospice and home care can meet these challenges.
We recognize that the AAPI community has diverse attitudes and practices surrounding illness, hospice, and death.
Although some AAPI practices are widely shared, such as respecting elders, using white and yellow colors, and burning incense, some practices vary. Chinese and Korean values can require the family to keep vigil by a dying loved one. The Chinese tradition, however, may maintain a hierarchy within the family structure, while the Korean tradition might maintain the division of genders. In other AAPI traditions, individuals, like expectant mothers, are discouraged from visiting someone at their end-stage of life for their own protection. In addition, some cultures place great value on a loved one being cared for in their own home at the end of their life.
Apreva Hospice understands that these spiritual practices can, and should be, honored. We’re here to accommodate by providing professional, competent, caring, in-home service that maintains sensitivity to these values.
Care goes beyond medical support. We are prepared to and can help you and your family with the hospice and bereavement journey with sensitivity toward AAPI’s religious, spiritual, cultural, and personal beliefs. This respect extends beyond rites and rituals and into practical care. The Native Hawaiian belief that spiritual essence (mana) is in all parts of the body can, for example, influence feelings about organ donation or cremation. But awareness of this belief informs our good care for a Native Hawaiian in the end stage of life.
The AAPI population is growing. By 2050, AAPI will become nearly 10% of the total United States population. It’s important that they can get the end-of-life care they need. Our staff ensures that everyone in our care, their family, and their loved ones are treated with respect.
Some Eastern philosophies view death as part of a cycle in which a loved one’s passage serves as a reminder to celebrate the miracle of life. Our team celebrates the lives of the people we care for, and what makes each of them unique. We’re proud to join this month’s celebration of Asian and Pacific Islander American Heritage Month. We invite interested AAPI Americans to learn about our hospice and in-home services, confident their culture and traditions will be honored.

By: Anonymous
We invite all community members to join us to recognize National Hospital Week, May 8 to May 14, 2022. Here’s more about this yearly observance and how we honor it at Apreva Hospice.
National Hospital Week is observed every year during the week that includes May 12, Florence Nightingale’s birthday. Florence Nightingale is best known for founding modern professional nursing and demonstrating the importance of nurses and their roles in the healthcare community.
Established in 1953 by the American Hospital Association, National Hospital Week highlights and recognizes hospitals and healthcare workers and the many innovative ways they support their communities.
Our team understands how challenging and demanding the hospital setting can be. We want to thank physicians, nurses, social workers, discharge planners, aides, and all other clinical staff members who have supported and cared for our patients and communities over the past year, especially given the unique ongoing challenges presented by the COVID-19 pandemic. Your hard work, long hours, and dedication to your communities have helped improve the quality of care for thousands of people in need.
As a leading hospice treatment provider, Apreva Hospice extends extra thanks to hospitals that partner with hospice providers. Your care and services have dramatically improved the quality of life for terminally ill patients and their families. In addition, you have given our team the opportunity to help these families save on hospital-related costs and deliver highly personalized care that helps them fulfill their loved ones’ final wishes.
We look forward to continuing our relationships with hospitals that partner with hospice treatment providers and are confident that together we can handle any unforeseen challenges that may come our way. In honor of National Hospital Week, thank you.

Some of the most common misconceptions about hospice care involve when it’s appropriate for a patient to elect hospice services and what diagnoses qualify a patient for hospice. People often assume hospice is only for cancer patients, but that is simply not true. You may be surprised to learn that stroke patients also qualify for hospice services.
Strokes are the number five cause of death and a leading cause if disability in the United States. A stroke is defined as a disease that impacts the arteries leading to and within the brain. It occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or ruptures. When this happens, part of the brain cannot get the blood and oxygen it needs, causing it and brain cells to die.
The American Stroke Association uses F.A.S.T to help us identify warning signs of a stroke.
If one side of the face is drooping or numb, this can be a common sign of a stroke. One way to help to determine this is by asking the person to smile. If their smile is uneven, that is an indication of face drooping caused by a stroke.
Another sign can be if one arm feels weak or numb. Ask the person to raise both their arms. If one arm drifts downward, it could be a sign of a stroke.
Slurred speech is a third sign of a stroke.
If someone is showing these three warning signs of a stroke, call 911 immediately.
Other signs and symptoms of a stroke can include:
Given the danger of strokes, it’s important to understand the different risk factors, including both those within and out of your control.
Some risk factors of stroke are within your control. These can include:
As with anything else, some stroke risk factors are beyond your control. These can include:
Hospice can benefit patients who are in the terminal stages of a stroke. The following criteria could be indicators that it may be a good time to consider the additional support of hospice.
If you are still unsure if your loved one qualifies for hospice, or if you have any questions about hospice for stroke patients, please don’t hesitate to contact us.
Volunteers are an essential part of the hospice care team. The difference they make for our patients and their families is immeasurable. Whether it’s through direct care or administrative work behind the scenes, there are countless ways a hospice volunteer can help.
We are beyond grateful for the incredible people who volunteer their time and talents to make a positive difference in our patients’ lives. In honor of National Volunteer Month, we’d like to recognize just a few of them. We asked our volunteers to share what made them decide to be a hospice volunteer and what they find most rewarding about their experience.
Hospice of the Midwest Volunteer – We Honor Veterans Program

“On September 10, 2018, Mr. Kelly Gafkjen, Chaplain, Hospice of the Midwest, was a guest speaker at our Urbandale-Johnston Veterans of Foreign Wars monthly meeting. Kelly was on a mission seeking veterans to talk to veterans in local hospice care in their homes or hospice facilities. Many veterans in hospice would like to share their life and military experiences, but feel only a fellow veteran can associate with their feelings. At the conclusion of his presentation, Kelly asked that we consider volunteering, receive some minimal training, and agree to talk to veterans who are seeking fellow veterans to talk to. After our meeting concluded, a number of us discussed the information presented by Kelly, and three of us thought this was right in line with our VFW mission of “Veterans helping Veterans”. Contact was made with Kelley and the three of us started our training at the Fall Training Session September 27, 2018 , conducted by Kelley and Taylor Schneider. By the end of October we had finished our training and were waiting for our first assigned veteran. Under the guidance of Taylor I was introduced to my first veteran during a pinning ceremony on November, 30, 2018. Since then I have had the privilege of meeting and sharing both civilian and military experiences with 9 veterans of WW II, Korea, Vietnam and the Cold War eras. Every veteran, whether Army, Air Force, Navy or Marine, were all comrades and had their own unique and fascinating stories to tell. Some sad, some humorous, but all seemed willing to share with enthusiasm. I so much enjoyed visiting with these men, and I only hope they felt the same comradery that I felt while in their presence. I will miss these veterans but look forward to meeting my next comrade.”

“Kendall and I (Ashley) love volunteering for Premier Hospice! We started in 2019 and volunteer weekly. Kendall states that he enjoys working in an office setting and learning new skills. I have been working with Kendall through the Medicaid Waiver program for almost 5 years. Seeing Kendall get to experience a work-type setting and learn new skills has been very rewarding. Nikki is a lot of fun to work with and always makes us feel appreciated!”

“We started volunteering for a local hospice during the pandemic (2020). We stumbled upon the opportunity from an email our mom received asking for donations of homemade casseroles and cards for hospice patients and their families. At first, it started by making occasional cards and casseroles, and then it turned into a routine every other week activity. This evolved into helping other hospices including including Grane Hospice. We have made homemade cards and even have given a virtual concert for the patients at Grane Hospice. We feel grateful to be able to give back to others in need even during a worldwide pandemic. It shows no matter what the circumstances, we can help others in our community. All this volunteer work has inspired us to create our own non-profit group called Rays of Sunshine, benefiting local hospices. We hope to expand and help even more local hospices in the future.”

“Coming from a family where both parents were in the medical field, I have had an interest in medicine ever since I can remember. In the pursuit of getting involved with medical volunteering opportunities, I wanted to commit to something that would provide meaningful experiences in vulnerable people’s lives, as well as my own. Although my patients’ physical bodies are failing them, they still have great wisdom to impart when given the chance to share and be heard. Many times, I leave the local assisted living facility with an enlightened perspective that I believe will serve me well in the career I am aspiring to have. From hearing first-person stories of World War II experiences to celebrating 96 years of living, there is always a window for valuable learning opportunities when I have the chance to spend time with these folks whom I now consider my friends.”
“I Prayed about being a Hospice Volunteer and this is how the Lord is using My ability as a Hairdresser, to bring Comfort and Joy to the Patients. The most rewarding aspect is seeing the Happiness in the Faces of the Patients and their Families. Working with Them is a Blessing to Me.”


“Being a hospice volunteer is about having a passion and love for helping others. No, I don’t physically help them but the most rewarding part about volunteering with my dog, Flynn, is seeing the joy it brings to residents. Residents look forward to our visits and remember us from week to week, allowing special connections to be made. I’m thankful for the opportunity Flynn and I have to give our time and make people smile.”

Kennedi and Ernest – graduate level social work students with Alabama A&M University and the University of Alabama – are student volunteers with Hospice of North Alabama in Huntsville. They sit with patients to provide caregiver respite. Hospice volunteer work allows students to garner a strong understanding of how social workers broker services within a healthcare agency as well as how to coordinate with various other healthcare and social service agencies.
Ernest states “I have learned that the process of dying and bereavement is as diverse as the families we serve. The first step of serving this population is engaging the patient and/or caregivers on what they want this time in their lives to be like—no two answers are the same.”
Along with the home environment, they also work with residential care communities to provide comfort and support. This gives them experience working with diverse community types and medical care needs.
Kennedi states “The things I’ve learned while interning at Hospice of North Alabama have prepared me to be a more caring and competent social worker. The compassion and kindness that HNA shows to the patients has been extended to me from the very beginning, and I’m so grateful. This has been the greatest experience of service I have committed myself to.” Ernest agrees, adding: “Knowing that you have provided support to a patient and/or their family in this transition period is rewarding. Establishing the trust that fosters comfort and emotional resiliency is an experience that will give volunteers a unique understanding of how health care best serves patients in all life stages.”
“My internship and volunteering experience with Premier Hospice was meaningful and fulfilled my longstanding desire of working with end-of-life services to clients and their families.
I enjoyed working with a well-resourced team that included a chaplain, bereavement coordinator, social workers, liaisons, nurses, a doctor, and a volunteer coordinator. Each of them brought to bear their own particular skillset, and we all collaborated to make our clients’ end of life as comfortable and dignified as possible.
Besides teamwork, I enjoyed, I enjoyed visiting with my client once a week. My primary role was to support and strengthen the care providers so that they might function better.
I also enjoyed supporting other team members by making caring calls to clients or their families. It was amazing how much comfort and reassurance I could bring to them through the calling service. My participation in the online bereavement group was my gain in the understanding and knowledge of the process in group work, particularly for grieving families.
Through my time with Premier Hospice, I have grown to better appreciate the important role of leadership in the hospice setting. The internship was profitable to my professional growth and development.”

“I volunteer with hospice to facilitate new transitions. In January 2020, I completed the training to become an End-of-Life Doula in New York City. In my move to Indianapolis, it was important for me to find a strong hospice program where I could be actively involved in the moments of life and death with others.
I volunteer because dying is an important cycle in every community. It is never easy to participate in the dying process, it pulls at every piece of your being. But there is nothing more rewarding than helping a patient or caregiver smile again while recalling a significant life moment. There is nothing more rewarding when the world feels burdensome, to help others find peace even for a single second.”
Thank you to these incredible individuals – and to all the volunteers on our team – for all you do for our patients and their families. You are amazing!
Interested in learning more about volunteer opportunities at Apreva Hospice? We’d love to have you on our team! Learn more and apply here.